Discover the symptoms and causes of stomach acid issues and how to manage them naturally.
Digestion is a top-down process.
With so much focus on probiotics, prebiotics, and other supports – it can be easy to forget about the potential need for stomach acid to jumpstart the digestive process.
Proper digestion, immune response, and a healthy microbiome depend on good acid production in the stomach – prior to the release of bile acids and pancreatic enzymes in the small intestine.
Hydrochloric acid, or HCl, helps increase the acidity of the stomach so that proteins can be broken down into smaller chains that can be absorbed.
The stomach lining also releases pepsinogen – which converts to pepsin from the acidity of HCl. Pepsin is responsible for physically chopping down proteins into individual amino acids and shorter peptides. HCl and pepsin work together. HCl initiates and greases the wheels. Pepsin then starts chopping proteins into smaller peptides and amino acids.
Later, peptidases in the small intestine will take these smaller peptide chains and chop them down further into their amino acids.
In addition, friendly microbes work together with other gastrointestinal secretions to digest fat, carbohydrates, fibers, and polyphenols.
The additional breakdown of otherwise non-digestible material creates and extracts new metabolites from our food that our gut, body, and brain use to optimize function. Researchers refer to the total production of unique metabolites as our “metabolome“.
The metabolome refers to the diversity of unique compounds your body has produced at any given time. I expand the definition to include all of the compounds the body is capable of producing when called upon. The more quantity and diversity of metabolites that you produce (or can produce in response to a stress) – the better able your body is to respond to stress and physiological needs on the spot.
The definition of health is the body’s ability to respond to an ever-changing environment.
Healthy digestion is necessary for a healthy microbiome.
A healthy microbiome is necessary for a healthy metabolome.
A healthy metabolome is what helps our body respond to its environment. In return, we digest future meals well and the cycle continues (See Image).
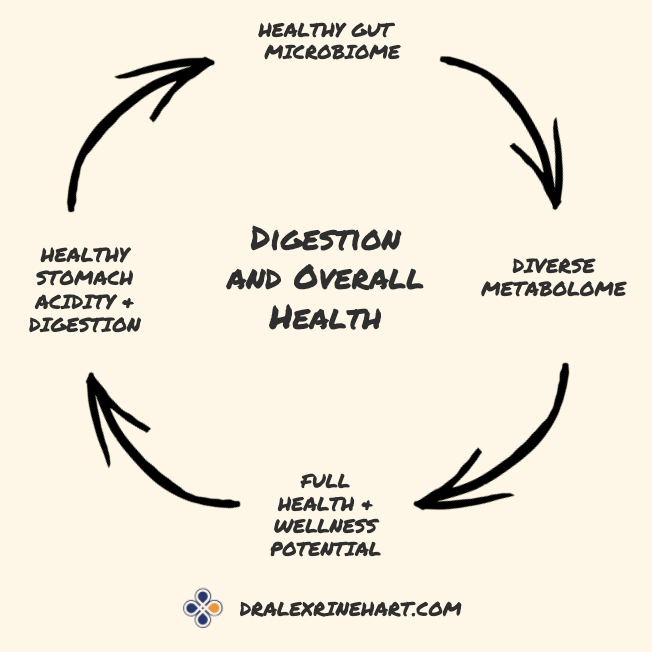
Digestion and Overall Health: Healthy digestive action promotes growth of healthy microbes and provides them with prebiotics they use as fuel. In return, microbes extract and produce metabolites (adding to the total “metabolome” of the body). The metabolome determines how well our body responds to physiological demands.
Our body uses the metabolites as “messengers” to respond to ever-changing needs. As a result, poor acidity and digestion in the stomach makes us less equipped to respond to the physical and metabolic stresses of life.
Up to 25% or more of the total metabolome (metabolites/messengers in our blood) is dependent on healthy gut flora.
Incomplete Digestion – A Problem for the Entire Digestive Tract
When digestion is incomplete – it creates stress further down the gastrointestinal tract.
- Low stomach acid and low pepsin activation disrupts the function of other digestive enzymes, bile acids, the ability for healthy bacteria to grow; and reduces our ability to yield the most benefit from the healthy activity of our gut microbiota.
- Low gastric acidity promotes the growth of unwanted microbes and the creation of their toxic byproducts that gunk up liver function, create inflammation, and contribute to body aches, brain fog, and fatigue. Low acidity increases the chances of infection by outside pathogens from the bacteria in our air, food, and mouth.
- All later stages of digestion are compromised when the initial steps in the stomach are botched. Low stomach acid refers to low release of hydrocholoric acid (HCl). When HCl release is low, it’s referred to as “hypochlorhydria”.
- Probiotics, prebiotics, and mucosal supports are important – yet, don’t forget about stomach acidity and digestive support. Use a Betaine HCl and Pepsin supplement, and/or take one tablespoon of apple cider vinegar diluted in 2oz of water directly before meals to acidify the gut, activate pepsin, and support later phases of digestion. Apple cider is also available as capsules to avoid tasting the vinegar. I like Apple Cider Vineger 500mg capsules by Natural Factors.
Symptoms of Hypochlorhydria/Low Stomach Acid:
 Digestive compromise can be experienced as bloating, or feeling like food is sitting heavy or like a rock in your stomach after eating.
Digestive compromise can be experienced as bloating, or feeling like food is sitting heavy or like a rock in your stomach after eating.
One might recognize food in the stool, your bottom may be itchy, and the stool may come out pencil-thin or poorly formed. You may experience reflux, constipation or diarrhea.
Isn’t reflux a sign of too much acid? Not so fast.
If it is low on acid production, your stomach may churn harder and splash the little bit of acid it does produce as high as the esophagus. The lining may be irritable and more sensitive to acid in the first place. Also, the lower sphincter of the esophagus can relax for a number of reasons when digestive health is compromised and this allows acid to splash.
Plus, if you’re not producing enough acid, food sits longer in your stomach.
So, when you eat at night and lie down to sleep or watch television at night with food heavy in your gut, the lack of gravity allows the acid to splash up. “Silent reflux” often occurs when you may not feel irritation, but acid is still gnawing at your lower esophageal lining nightly if you’re eating too late. You can aim to stop eating three hours before your intended bedtime to prevent this from happening.
You may also notice an occasional metallic taste in your mouth or bad breath. Burping and excessive gas may develop. Your hair and nails may be more brittle and lose their normal luster.
These are all signs of low stomach acid and poor protein breakdown.
Now, let’s look at what causes this to occur…
Causes of Low Stomach Acid:
-
Poor nutrient status
Zinc and magnesium are the biggest players that support stomach acid production. They are also common deficiencies due to stress and immune overload. I use Zinc Copper Balance or Zinc Carnosine to support zinc and magnesium glycinate for magnesium.
Often, clients are taking zinc carnosine to support mucosal health and it also supports zinc status at 16mg of elemental zinc per serving. Be mindful of how much zinc is in your combined supplements as intakes above 30mg can start to contribute to nausea.
You also want to balance a high intake of zinc with copper(generally 1mg copper for every 15mg of Zinc) if copper is not included in your zinc supplementation.
-
Helicobacter pylori (H. pylori) overgrowth
When overgrown, H. pylori degrades the stomach lining, reducing the ability to produce acid – and making the stomach irritable to the acid it does produce.
H. pylori also produces toxic factors like ammonia and acetaldehyde (a byproduct of alcohol that gives high alcohol consumption its toxic effect) (1). A Nobel prize was awarded to Barry Marshall for the discovery of H. pylori and its link to gastritis and peptic ulcer disease.
Before Marshall’s discoveries, stomach cancer was a leading cause of cancer deaths.
While medical therapy is sometimes needed, natural support options for H. pylori include PyloGuard by Microbiome Labs, licorice flavonoids known as “Gutgard” in MegaGuard, mastic gum, and antimicrobial herbs like those found in Berberine Reset by Doctor Alex Supplements, G.I. Microb-X by Designs for Health, Olivirex, or Oil of Oregano.
Because H. pylori irritates the lining of the stomach, the mucosa-supporting herbs and compounds in GI Revive can be supportive as well as zinc carnosine.
-
Overuse of acid-blocking medication (H2 blockers, proton-pump inhibitors/PPI’s) or over-the-counter digestive aids
When acid production is blocked, one no longer benefits from the digestive, absorptive, and pH-supportive functions of stomach acid.
Acid-blockers are not intended for intake over months and years. Yet, this is exactly the case for thousands of individuals. When taking these medications, you block acid production and feel better – but functionally, you’re doubling down on the disadvantages of low stomach acid long-term.
A doctor may recommend H2 blockers or PPIs over the short term to allow significant stomach irritation to heal.
Ideally, due to the long-term effects of acid-blockers, the medication should provide a window of relief while one actively seeks alternative solutions to address the causes of the dysfunction in the first place. Too few seek those alternative solutions.
The other problem comes when discontinuing the drugs after months or years of use. When discontinuing acid blockers – a weaning off may be needed as you can experience a severe rebound in acid production upon discontinuation.
The body’s production goes into super-compensation when the drug is first removed.
While normal, this rebound can be misperceived as your original symptoms coming back (when they may be coming from the drug withdrawal). Often, this means a person will return to further use of the medication.
Drug withdrawal could be its own separate cause of stomach acid issues.
Work with your prescribing doctor with your questions and concerns and personalize a plan when using these medications and create a plan for coming off of them when you’re ready.
-
Brain or nervous system inflammation or trauma
This is one of the most overlooked areas of slow digestive function.
Trauma in the nervous system (brain/spinal cord) can affect the function of the other nervous systems: the sympathetic nervous system (stress balance) and the enteric nervous system (gut function).
Trauma includes head injuries and concussions, but also inflammatory reactions that injure the central, enteric, and peripheral nervous systems.
These nervous system reactions can come from infection (EBV, H. pylori, others), mold (food and home sources), food (especially wheat), metals (ex/ arsenic, mercury, cadmium), pesticides (glyphosate, PCB’s), and pollutants (formaldehyde, fire retardants, benzene, off-gassing from electronics, glues, and processed construction materials).
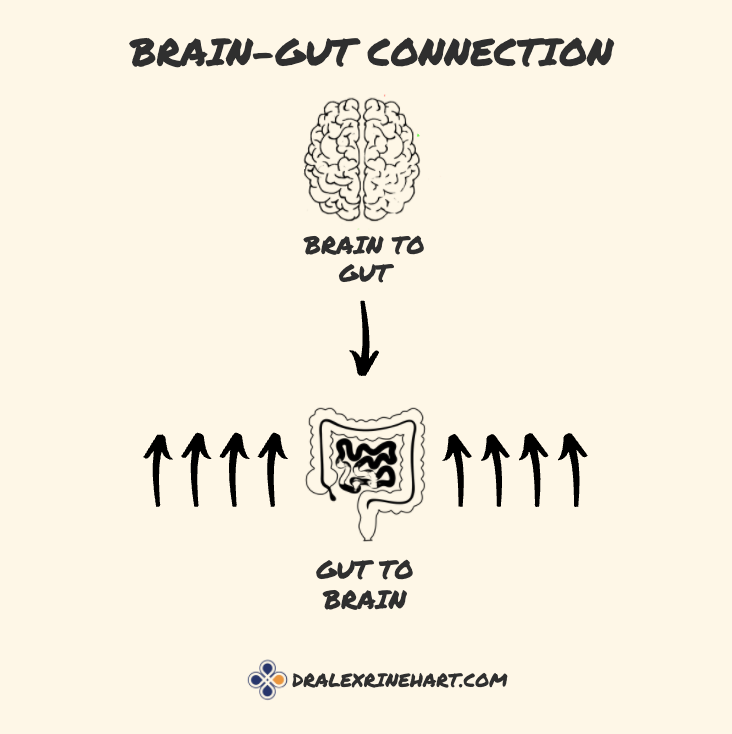
When you look closer at the gut and brain connection. It’s a weighted relationship – the gut affects brain function much more strongly than the reverse. There are eight messages going from the gut to the brain for every one pathway from the brain to the gut.
When you have an immune reaction to gluten, it is 8x more likely to manifest as brain and nervous system issues than gut symptoms! Cases like these may be described as “silent celiac disease” or non-celiac gluten sensitivity.When someone is sensitive to gluten (wheat, rye, barley), the symptoms are eight times more likely to manifest in the nervous system than the gut with symptoms ranging from poor focus, forgetfulness, fatigue, brain fog, insomnia, anxiety, depression, loss of balance and coordination, loss of taste or smell, and other neurological signs and symptoms including peripheral neuropathy.
If you carry any “slow” gene variations in the HLA DQA2 and DQA8 genes, I personally recommend proactive elimination of gluten from your diet, or at the least, annual testing of wheat antibodies using a test such as Array 3 by Cyrex Labs. If any antibodies show up, it’s time to eliminate sources of gluten from the diet and evaluate cross-reactive foods. You can measure antibodies to cross-reactive foods with Array 4 by Cyrex labs.
When it comes to Cyrex testing, ask your doctor to order a kit for you, or find a functional medicine practitioner who is more likely to provide the testing for you. If you run out of local options, contact us with your name and intended shipping address and we may be able to help.
Gluten causes leaky gut in ALL who consume it because humans do not make the DPP-IV enzyme that is necessary to break it down. This occurs whether you have an immune reaction (IgG, IgE, IgA antibody reactions) or not!
If you eat wheat, react, and also carry HLA gene variants mentioned above, the reaction to wheat can also include a much stronger and damaging T-cell immune response that can damage the intestines or nerve tissue more severely, in addition to any IgG, IgE, or IgA reactions.While I recommend most people follow a gluten-free diet, that recommendation is much more definitive for those who carry HLA gene variants.
For others who choose to consume wheat, I recommend no more frequently than once every four days so that your gut has time to react and heal before your immune system ratchets up reactions on top of one another with frequent intake.
Doctors who work with neurological cases frequently report complete resolution of the spinal cord or multiple-sclerosis-like symptoms when clients remove gluten completely from their diet. The rub is that neurological symptoms can take decades to manifest – but the cause (such as long-term gluten intake) can start decades earlier. Nerves in the brain and spinal cord do not have pain fibers – meaning your only measure of a problem is loss of function – and this loss of function can take years.
The good news is that early dysfunction can recover in weeks and months.
Brain circulation support (NeurO2 by Apex Energetics), and gluten-free/dairy-free eating are baseline strategies for any nervous system trauma.
A number of other nutrients and botanicals support nerve function but some of my favorites are phosphatidylcholine powder, palmitoylethanolamide (PEA), lion’s mane mushroom, and curcumin.
Stress-supportive strategies may also be supportive and many botanicals overlap with benefits for neurology too. Phosphatidylserine is a staple to stress-reducing strategies – I use a transdermal phosphatidylserine source called Adrenacalm or Adrenastim to support stress balance. Adrenacalm SE or Adrenastim SE are unscented versions that leave out the essential oils for those with skin irritation to essential oils or who are sensitive to smells.
Adrenastim is best for morning or early afternoon use for more progressed fatigue and those who tend to low blood pressure and orthostatic hypotension (dizzy when you stand up too fast). Adrenastim is also generally contraindicated for those with high blood pressure due to the licorice root – but you can work with a functional health doctor to know what’s right for you.
Adrenacalm can be morning, afternoon, and evening support.
Check with your doctor if you are taking any antidepressant medication as Adrenacalm contains St. John’s Wort (which while widely known as a mood/serotonin support, is also a “nervine” herb that supports the nervous system and immune health).
I also like the combination powder of Phosphatidylcholine and Phosphatidylserine power by Interplexus and mix in smoothies so that the flavor is not so direct on its own.
Another overlooked and more expensive treatment strategy is neurofeedback – which analyzes brain wave patterns and personalizes training to coax brain wave patterns back into balance following stress or trauma.
Hypobaric oxygen chambers can be available at an office near you and also support faster healing.
Red light/infrared therapy (link to the device I use) helps stimulate healing and recovery on a cellular level and can support brain function and the health of your circadian rhythms which are important for both brain and gut function.
This circadian rhythm of the gut is under-appreciated – which brings us to the 5th cause of low stomach acid…
-
Digestive overwork from overeating (or over-drinking) in quantity, timing, or frequency

Overwork can result from suboptimal meal timing, poor sleep patterns, and late-night eating.The gut has a “circadian rhythm” to it – meaning it cycles between periods of activity and necessary rest. Without rest, you’ll fatigue the release of digestive juices, and bile flow can start to sludge up too, slowing not only fat digestion but also the ability of bile salts to bind and detoxify hormones and toxins.
Sleep studies have shown that eating within three hours of the intended bedtime negatively affects sleep quality. Your gut needs to “turn off” for the night and modern lifestyles do not always allow this to occur.
Intermittent fasting (IF) of 12-16 hours helps give the gut a necessary break to finish its work from the day – and is associated with a myriad of other metabolic benefits and can help spur microbiome diversity. If you stop eating at 8 pm, your first meal the next day may not be until noon the next day.
Intermittent Fasting is one of my favorite strategies, as it only changes the time you eat and can be easy and affordable to implement.
-
Leaky gut
When the gut is leaky from eating allergic or sensitive foods or from other sources of inflammation – you absorb endotoxins – most notably Lipopolysaccharides (LPS).
LPS causes inflammation in the nervous system that can create metabolic trauma to nerves – but it also can “turn off” or “block” motility at the level of the central nervous system (brain and spinal cord). You can take digestive aids such as ginger and motility aids like MotilPro, but if they’re not doing the job, it’s time to address LPS and leaky gut.
Food sensitivities, allergies, and intolerances (gluten, dairy, and others) will put more strain on your system and cause local inflammation that can directly irritate mucosal linings, cause leaky gut, and contribute to systemic inflammation due to leaky gut and endotoxin absorption.
Other barrier systems can become leaky – specifically the brain-blood barrier and the lung barrier. So the same factors that trigger a leaky gut can cause a leaky brain or leaky lungs. Air quality is just as important as food quality.
The lungs and gastrointestinal system are the primary interfaces between the outside world and our inner body – they are vulnerable to irritants, inflammation, and stress.
MegaIgG2000 contains immunoglobulins that help to bind and neutralize LPS as well as other toxins and is a common tool for leaky gut in addition to Megasporebiotic and other supports.
Megasporebiotic has been shown clinically to reduce endotoxin release by as much as 40%.
I carry my own spore probiotics mix called Sporeboost IG that has spore strains with added IgG to support the binding of endotoxins.
-
Aging
We naturally produce fewer digestive enzymes as we age, especially pepsin. Some refer to this as an “enzyme reserve” that naturally runs out with older age.
With each passing decade – we benefit more from “top-down” digestive support – and digestive support will help us maintain our enzyme reserve and slow down its decline. As a result, one can slow sarcopenia (muscle wasting) with age as one continues to absorb proteins optimally.
Taking enzymes can be a proactive wellness habit and longevity strategy and doesn’t need to be triggered by a gut complaint. Sooner or later, all of us could benefit from acid and pepsin support in the gut.
So while the next section discusses how to support stomach acidity and protein digestion, it’s important to address the underlying causes listed above to stay ahead of the issue in the first place!
Now, let’s learn what we can do about low stomach acid…
Acidifying the Stomach Naturally for Digestion, Microbiome Balance, and Healthy Aging

The production and release of hydrochloric acid and pepsin in the stomach naturally decline with age.
First, the causes of low acid production accumulate with age.
Older adults are more likely to deal with H. pylori or low magnesium levels or have just had more years of combined stomach irritation blocking the normal production of stomach enzymes.
Second, while healthy elderly adults may still produce enough acidity in their gut, their ability to release pepsin does physically “run out” with age (2; 3).
Your body has somewhat of a set amount of pepsin it can release before it runs dry – similar to an engine having a certain amount of revolutions before its life runs out.
Ideally, this means every adult over the age of 70 should be taking a betaine HCl and pepsin supplement to support protein digestion.
And, this means we can start earlier in our 40s and 50s with support to optimize stomach secretions long-term.
Additionally, the more you can address the causes mentioned above – the less likely your stomach lining will be subject to gastritis and the physical breakdown of the cells responsible for releasing secretions.
Betaine HCl helps acidify the stomach and activate pepsin. Pepsin is responsible for physically chopping up protein. The acidity is crucially important for the microbiome as well – the acidity in the stomach promotes proper pH balance in the rest of the intestines – which makes sure the right bacteria are growing where they need to be – while blocking the growth of the wrong microbes.
A strongly acidic stomach is another means of protecting the body from opportunistic pathogens – especially when we breathe in microbes, or swallow saliva and its oral (and sometimes fecal) bacteria.
Pepsin requires a low pH (high acidity) to function best – so both HCl and pepsin are typically taken together.
I use DigestStart – Betaine HCl and Pepsin as my preferred source of supplementation. I also use apple cider vinegar before meals – and for those who do not like the taste, Natural Factors makes apple cider vinegar capsules.
Apple cider vinegar also supports acidification of the stomach and activation of pepsin. Pepsin is commonly combined with the acidifying property of betaine HCl in supplements – but apple cider vinegar may be more affordable long-term and you might get away with a lower dose of an HCl/pepsin supplement by combining the strategies.
Fermented foods contain enzymes, organic acids, and acidity too.
A little goes a long way, sometimes just a spoonful of fermented food is enough without causing other potential issues with histamine or overstimulation of the immune system from Lactobacilli probiotics. Histamine intolerance and Lactobacilli overgrowth can be more common for those with long-standing issues with stomach acid.
Lactobacilli are a common group of strains in yogurts and other fermented foods. They are a concern, especially for those with small intestinal bacterial (SIBO) or fungal overgrowth (SIFO). SIBO/SIFO is one of the many possible consequences of low stomach acid.
So, by all means, you can use 1-2 tablespoons of apple cider vinegar diluted in 2oz of water (shot glass amount) OR take apple cider vinegar capsules shortly before a meal to acidify the stomach or take a spoonful of your favorite fermented food.
Another strategy that can be used is to take digestive bitters – the bitter flavor primes the engines below to start churning out secretions.
As you get older, you may benefit more from direct HCl and pepsin support as your ability to produce pepsin declines naturally!
How to Take Betaine HCl and Pepsin Correctly
Betaine HCl intake instructions can be important to see results.
First, you may want to dose while under the management of a functional health doctor.
If your stomach lining is thin, irritated, or you’re simultaneously taking a lot of NSAIDs like ibuprofen or acetaminophen, other strategies (such as bitters, and gut lining support) may be better for you when first starting.
It’s also useful to evaluate all causes of dysfunction, not just stomach acid, and a functional medicine doctor can identify those triggers for you. I’m not in the business of seeking silver-bullet fixes to global digestive issues.
For those ready to take the plunge, start with 1 capsule of Betaine HCl with a high-protein meal. Take it after the first few bites of food. Try it for 2-3 days and evaluate if it causes extra “warming” in your belly. If it does, this is a sign that you’re producing enough stomach acid.
If not, move up to 2 capsules for a few days, then 3, and you may need to work up to as much as 7 capsules. The form we use is 496mg of betaine HCl, so we would normally stop as high as 7 capsules and not exceed 3500mg. The goal is to find the point where you feel the warming, and reduce your intake by one capsule. If you’re not noticing the warming, more extensive support may be needed instead of increasing capsules further.
Many people find that the level of their need may go as high as 3500mg early on – but start low and work up to that point as discussed above.
It might take 2 capsules, it might take 7, and the dose will vary per individual. It’s better to take some than none, so the affordability of dosing may also dictate how high you’re willing to go for large protein meals.
As your acid production improves, it will take less betaine HCl to trigger the warming and you’ll be able to take fewer capsules.
You can take less in line with the serving size of protein. Generally, you want to “test” with meals that contain at least 20-25g of protein in the serving.
If you take a bunch of capsules with a low-protein meal, you can experience warming and it’s likely more of an indication of the low protein level being consumed. You still may not produce enough acid for larger protein meals.
If you’re not noticing improvement – it’s time to evaluate the list of causes again to see if there’s something missing in your approach.
You may need to spend some time cooling off inflammation and supporting the stomach and gut linings prior to starting acid support in the gut.
Digestion is a top-down process and the health and stability of the gastrointestinal system require strong acidity in the stomach at the start.
Use the strategies above to optimize acid production and promote good digestion.
Related Links:
-Heal the Gut Lining and Leaky Gut Naturally
–Polyphenols – Next Generation of Prebiotics
-Intermittent Fasting on Gut Microbiome
-How to Measure the Health of the Gut Microbiome – Personalized Microbiome Analysis
-Anti-Aging Benefits of Intermittent Fasting
-The Megasporebiotic Leaky Gut Study
-The Megasporebiotic and Megaprebiotic Synbiotic Study
-How to Stop Toxins from Leaking into Your Blood
-SIBO
-Taking Probiotics
-The Ultimate Guide to Megasporebiotic
-Enviroklenz

